Essential Facts About Covid-19
By James D. Agresti
December 13, 2020
Updated 5/12/23
Overview
Given the spread of misinformation about Covid-19, Just Facts is providing a trove of rigorously documented facts about this disease and its impacts. These include some essential facts that have been absent or misreported in much of the media’s coverage of this issue.
This research also includes a groundbreaking study to determine the lethality of Covid-19 based on the most comprehensive available measure: the total years of life that it will rob from all people. This accords with the CDC’s tenet that “the allocation of health resources must consider not only the number of deaths by cause” but also the “years of potential life lost.”
While stating that the “ongoing investigation” of Covid-19 is still “a rapidly evolving situation,” the CDC stopped reporting active Covid cases and aggregate deaths on May 11, 2023, shortly after the World Health Organization declared an “end to the public health emergency.” Prior to then, Just Facts methodically updated the emboldened figures in this article with the latest CDC data on cases and deaths. Other facts that informed the broader picture were updated or added on a periodic basis.
On one hand, these facts show that:
- the average death rate for people who contract Covid-19 is well below 1% and is much closer to that of the seasonal flu than figures that were commonly reported by the press.
- the average years of life lost from each Covid-19 death are significantly fewer than from common causes of untimely death like accidents and suicides.
- the virus that causes Covid-19 is “very vulnerable to antibody neutralization” and has very limited ability to mutate, which makes it unlikely to take masses of lives year after year like the flu and other recurring scourges.
-
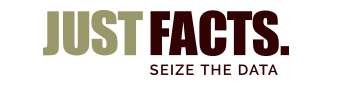
if two million Covid-19 deaths ultimately occur in the United States, the disease will rob about 26.4 million years of life from all Americans who were alive at the outset of 2020. In contrast:
- the flu will rob them of about 35 million years.
- suicides will rob them of 132 million years.
- accidents will rob them of 409 million years.
On the other hand, elderly people and those with chronic ailments are extremely vulnerable to Covid-19, and the disease is highly transmissible. This causes it to spread like wildfire among people with weakened immune systems or inadequate immunity to the virus which causes Covid-19 (SARS-CoV-2).
However, measures to limit the spread of C-19 sometimes involve fatal tradeoffs, and thus, overreactions can destroy many more years of life than they save.
Just Facts asked Dr. Rodney Sturdivant—who holds a Ph.D. in biostatistics and is the Director of the Statistical Consulting Center at Baylor University—to critically review this research. He assessed it as follows:
Likelihood of Exposure
Brooklyn, NY, May 24, 2020 (iStock via Kirkikis)
According to the U.S. Centers for Disease Control and Prevention, a total of 104,618,931 cases of Covid-19 have been reported in the U.S. as of May 3, 2023. Given that the population is 335 million people, this amounts to one out of every three people in the United States. C-19 cases are not equally dispersed throughout the nation, so this figure is much higher in some areas and much lower in others.
Nevertheless, the current likelihood of being exposed to C-19 doesn’t depend on the number of people who have ever been infected—but on the number of people who are currently infected and contagious. Determining this is confounded by three key factors:
- Symptoms of C-19 typically don’t appear until 2–14 days after exposure, which means that people can be infected for days or weeks before having any reason to get tested.
-
The vast majority of people who contract C-19 develop only mild symptoms or none at all, and hence, they may never be diagnosed while they are infectious. Despite widespread anxiety over C-19, medical studies have been clear from early on that it poses such a minor threat to most people that they may barely know they have it:
- In one of the few cases where asymptomatic cases could be reliably counted because an entire population was tested for C-19, Japan’s National Institute for Infectious Diseases reported in February 2020 that 51% of the people on the Diamond Princess cruise ship who tested positive for C-19 had no symptoms, even though the “passengers onboard were generally of an older age.”
- In another case where asymptomatic cases were reliably counted, the New England Journal of Medicine reported in April 2020 that universal Covid-19 testing of pregnant women at two New York City hospitals found that 88% of them who tested positive for the disease were asymptomatic upon admission, and 9% later developed a fever. Fevers are relatively common after childbirth, which means they were not necessarily from C-19. Accounting for both possibilities and the sampling margin of error, these results amount to a 65% to 99% asymptomatic rate with 95% confidence.
- A study published by the journal Clinical Infectious Diseases in October 2020 found that only half of elderly blood donors in Denmark who had antibodies for C-19 “reported having been sick since the start of the pandemic.” This indicates that the C-19 asymptomatic rate for elderly blood donors—who are typically healthy—is about 50%. Furthermore, an August 2020 paper in the journal Cell found that the number of people who have had C-19 is “probably significantly higher than antibody tests have suggested.” This implies that the asymptomatic rate for healthy elderly people is even greater than 50%.
- A study published by the journal Clinical Infectious Diseases in November 2020 estimated that only 13% of all C-19 cases that occurred in the U.S. from the outset of the pandemic in March 2020 up through September 2020 were “recognized and reported.”
- Perhaps most tellingly, the journal BMJ Thorax published a study in May 2020 about an outbreak of C-19 during an Antarctic cruise where everyone onboard “had no outside human contact” for 28 days. The passengers were quarantined in their rooms on the eighth day of the cruise, the crew wore personal protective equipment thereafter, and everyone was tested for C-19 on day 20. Among the 128 people who tested positive, 81% ultimately had no symptoms, 13% had mild symptoms, and 6% had serious symptoms, including one that died.
-
There are significant differences in the contagiousness of people infected with C-19, depending on whether they are symptomatic, pre-symptomatic, post-symptomatic, or asymptomatic. This reality has been shrouded in many publications because researchers often misuse an indicator called “viral load” to determine if people can transmit the virus.
In the context of Covid-19, viral load is the concentration of the virus’ genetic material detected in body fluids. The Journal of Clinical Virology notes that this measure has been “widely used” in C-19 studies “as a proxy for contagiousness,” but a German medical journal explains that the mere detection of genetic material “does not imply presence of viable and replicating virus.”
In other words, the virus may be dead or unable to reproduce because the person’s immune system has neutered it. The German journal adds that researchers commonly use viral load to measure contagiousness because it is “convenient,” while the proper method is “cumbersome.”
The implications of using a convenient measure instead of an accurate one are evidenced by the fact that an August 2020 paper in JAMA Internal Medicine found that C-19 viral loads “were similar” in people during different stages of the disease—but studies that actually measure contagiousness show major disparities in their capacity to transmit infections:- An April 2020 paper in the journal Nature reports that live C-19 viruses could be “readily” cultured from the mucus of people with “mild” C-19 “during the first week of symptoms” but not “after day 8 in spite of ongoing high viral loads.”
- An August 2020 paper in the journal Nature Medicine estimates that 1% of C-19 transmission occurs more than 5 days before symptom onset and that infectiousness peaks at symptom onset and then declines “quickly within 7 days.”
- A related August 2020 paper in the journal Nature Medicine explains that worries about widespread transmission of C-19 by asymptomatic and pre-symptomatic people stemmed from models, and real-world observations from “direct contact tracing studies” have proven that the actual threat is “lower than that predicted by Covid-19 transmission models.”
- A contact tracing study published by the journal Respiratory Medicine in August 2020 found that none of the 455 people who were exposed to an “asymptomatic Covid-19 virus carrier” caught the disease, even though each of them were exposed for an average of 4–5 days. The paper thus concludes that “the infectivity of some asymptomatic” C-19 virus “carriers might be weak.”
- A contact tracing study published by the Annals of Internal Medicine in August 2020 found that merely one among 342 people who had “close contact” with asymptomatic C-19 virus carriers caught the disease from them. Based on this and other data, the study determined that the contagiousness of asymptomatic C-19 carriers is 91% lower than those with mild symptoms and 95% lower than those with moderate symptoms.
- A meta-analysis published by the journal JAMA Network Open in December 2020 found that less than 1% of people with asymptomatic or pre-symptomatic Covid-19 infect other members of their households. In comparison, the study found that 18% of people with symptomatic C-19 transmit the disease to their housemates, even though people generally take precautions around others who are symptomatic. These results led the authors to remark that “the lack of substantial transmission from observed asymptomatic index cases is notable.”
- A study published by the Canadian Medical Association Journal in April 2021 found that children who “tested positive for SARS-CoV-2 were less likely to grow virus in culture” than adults, “suggesting that children are not the main drivers of SARS-CoV-2 transmission.”
Applying the facts above and related data from the CDC and the Center for Evidence-Based Medicine at Oxford University, Just Facts developed a methodology to estimate the number of people in the U.S. who currently have infectious cases of Covid-19. The calculations—which are detailed in this spreadsheet—find that roughly one of every 1,407 people in the U.S. is contagious as of May 3, 2023.
Again, this is a national average and is not applicable everywhere because of large differences in the timing and severity of the pandemic in different areas of the country.
Deaths
iStock/Tempura
Fatal interactions between Covid-19 and other ailments like heart disease and diabetes make it difficult to determine the exact death toll from C-19. A range of evidence suggests that the CDC’s tally of Covid-19 deaths is inflated but still provides a reasonable measure of the pandemic’s severity.
According to the CDC’s estimate of “confirmed and probable” fatalities from Covid-19, the disease has played a role in the deaths of 1,131,819 U.S. residents as of May 3, 2023. To put this figure in perspective:
- it amounts to one out of every 296 Americans since the pandemic began in March 2020, whereas one out of every 116 Americans die every year.
- an average of 37,000 people per year died from the flu over the previous nine years.
- around 170,000 people die from accidents every year.
In comparative terms, average annual deaths involving Covid-19 since the outset of the pandemic are:
- 87% below annual fatalities from all causes.
- 9.6 times annual fatalities from the flu.
- 2.1 times annual fatalities from accidents.
Although C-19 is a new disease and took its first reported life in the U.S. during February 2020, these comparisons may substantially overstate its deadliness. This is because fatalities from accidents, the flu, and other common causes of death occur in droves every year, and this is unlikely for C-19 because of the facts below.
Immunity
Stockholm, Sweden, April 1, 2020 (TT News Agency/Fredrik Sandberg via Reuters)
The primary reason why the flu kills tens of thousands of people every year is that the viruses that cause it mutate in ways that prevent humans from becoming immune to them. Per the Journal of Infectious Diseases, “All viruses mutate, but influenza remains highly unusual among infectious diseases” because it mutates very rapidly, and thus, “new vaccines are needed almost every year” to protect against it.
In striking contrast, a March 2020 paper in a molecular biology journal that cites Michael Farzan, co-chair of the Department of Immunology and Microbiology at Scripps Research, explains that once a potent vaccine for Covid-19 is developed, it “would not need regular updates, unlike seasonal influenza vaccines.” This is because part of the virus “is protected against mutation” by a feature of its genetic material, or RNA.
The same point applies to naturally acquired immunity. People who catch C-19 and other infectious diseases with low rates of mutation typically develop enduring resistance to them. The physiology textbook The Human Body in Health and Illness explains that such immunity, which is called “active immunity,” is “generally long lasting.”
For example, a study published by the journal Nature in 2008 found that survivors of the 1918 influenza pandemic still had immune B-cells that actively produce “highly functional, virus-neutralizing antibodies” that guard against the disease roughly 90 years later. Scientists were able to extract these B cells from the subjects’ blood and use them to generate monoclonal antibodies, which had “exceptional virus-neutralizing potency and protected mice from lethal infection.”
This is also the case with rubella, mumps, measles, and polio. After people contract these diseases and recover, they rarely suffer from them again or transmit them to others. Thus, they become firewalls against the spread of these contagions.
Media outlets like The Atlantic, Vox, and Forbes have turned the truth of this matter on its head by confusing the general nature of coronaviruses with that of C-19. The habit of calling Covid-19 “the coronavirus” can be very misleading because there are different types of coronaviruses, and C-19 is caused by just one of them.
Coronaviruses are a family of RNA viruses that include some common cold viruses which tend to mutate rapidly, but the virus that causes C-19 does not share that trait. Per the molecular biology paper cited above, the virus that causes C-19 “does not mutate rapidly for an RNA virus because, unusually for this category, it has a proof-reading function” in its genetics. The paper also explains that the same physical feature of the virus that makes it so contagious also makes it:
Simply put, the virus that causes C-19 is immunologically fragile, and thus, it is far less likely to take lives regardless of acquired immunity and vaccines. If this proves true in the long run—as all available evidence suggests it will—the lifetime risk of dying from Covid-19 is greatly overstated by comparing its current death toll to yearly fatalities from the flu, accidents, suicides, and other common causes of death. This is because the vast bulk of people will develop immunity to C-19 either by catching it or through vaccines. In vivid contrast, societies don’t become immune to accidents, the flu, or heart disease.
All of the above facts about immunology in general and C-19 in particular were published in medical journals, textbooks, or encyclopedias near the outset of the pandemic in March 2020 or earlier. Yet, the World Health Organization sowed confusion around this issue by publishing a scientific brief and a tweet on April 24th that stated, “There is currently no evidence that people who have recovered from #COVID19 and have antibodies are protected from a second infection.”
Many media outlets parroted that claim, even though the World Health Organization deleted its tweet later that day and wrote, “Earlier today we tweeted about a new WHO scientific brief on ‘immunity passports’. The thread caused some concern & we would like to clarify: We expect that most people who are infected with #COVID19 will develop an antibody response that will provide some level of protection.”
That clarification was closer to the truth but still misleading because it ignored these three key facts that were already proven by that time:
- The virus that causes C-19 has low mutational capacity.
- The virus that causes C-19 is very vulnerable to antibody neutralization.
- Viruses with these attributes are easy to protect against because naturally acquired immunity commonly provides long-lasting resistance to them.
Since April 2020, a torrent of research has confirmed those facts. This includes at least 20 studies which have found evidence that naturally acquired immunity to Covid-19 is potent and lasting. Some examples include the following:
- In May 2020, the South Korean CDC published a study of 285 people who contracted C-19, recovered, and then tested positive again. Contrary to the assumption that they must have caught the disease a second time, viral culture testing was performed on 108 of the subjects, and “all had negative results.” Also, “no case was found” in which someone “was newly infected solely from contact with” one of the people. These facts indicate that the positive C-19 tests were caused by remnants of dead or harmless virus particles. Thus, South Korea changed its policy to treat such individuals as non-infectious.
-
In August 2020, the journal Cell published a study of the immune system responses of 206 people in Sweden who had contracted C-19. Unlike other studies that only tested for antibodies, this one measured “T cells,” which are the body’s main source of “long-term immune protection.” This is important because antibodies quickly wane after infections, while T cells provide lasting immunity. The study found that:
- 100% of the subjects who had severe C-19 and 87% who had mild C-19 had “highly functional memory T cell responses, suggesting that natural exposure or infection may prevent recurrent episodes of severe Covid-19.”
- “In line with these observations, none of the convalescent individuals in this study, including those with previous mild disease, have experienced further episodes of Covid-19.”
- In August 2020, after Covid-19 had impacted “over 23 million patients with more than 0.8 million deaths in over 200 countries,” the journal Clinical Infectious Diseases reported the first proven case of someone catching C-19 and then catching it again. This sometimes occurs with all infectious diseases because immunity is not an all-or-nothing phenomenon, and it can be compromised by medical conditions or factors as common as poor sleep, excessive alcohol, psychological stress, obesity, or old age.
- In February 2021, the European Journal of Clinical Investigation published a paper analyzing all reported cases of C-19 in Austria during the first two waves of the pandemic. It found that people who caught C-19 during the first wave developed a degree of immune protection to the second wave “comparable with the highest available estimates on vaccine efficacies.” The study also found that no one who recovered from C-19 in the first wave died from it during the second wave.
- In June 2021, the journal Nature published a study of 63 vaccinated and unvaccinated people who recovered from Covid-19 and were monitored for a year thereafter. It found that “in the absence of vaccination,” the subjects developed B cells that remained “relatively stable” in number and actually developed “increasing potency and breadth” during “6 and 12 months after infection.” In the words of the paper, these findings “suggest that immunity in convalescent individuals will be very long lasting” and provide protection “against a wide group of variants.”
- In November 2021, the New England Journal of Medicine published a study of 353,326 people in Qatar who had been infected with C-19 from February 2020 through April 2021 while the Alpha and Beta variants were circulating. The study found “no cases of critical disease” and “no cases of death” among any of the people who were previously infected.
- In November 2021, the journal Infectious Diseases published an analysis of “well conducted biological studies” about naturally acquired immunity in a massive biomedical research database. It found that “multiple epidemiological and clinical studies, including studies during the recent period of predominantly delta … variant transmission, found that the risk of repeat SARS-CoV-2 infection decreased by 80.5–100% among those who had had Covid-19 previously.”
It is important to realize that immunity is not an all-or-nothing phenomenon, and scientific journals draw distinctions between:
- “clinical immunity,” defined by a 2009 paper in the journal PLoS as an immunity that “reduces the probability that an individual will develop clinical disease.” Notably, this doesn’t prevent infections but limits their harmful impacts by killing the pathogens before they do serious harm.
- “sterilizing immunity,” defined by a 2016 paper in the journal Scientific Reports as “a unique immune status, which prevents effective virus infection into the host.” The paper emphasizes that this is “different from” clinical immunity that “allows infection but with subsequent successful eradication of the virus.”
Time will tell more about the mutations of the virus that causes C-19, but current indications are that it will not dramatically mutate and become an ongoing cause of numerous deaths.
Years of Lost Life
Photo credit: iStock/kupicoo
Beyond raw numbers of deaths, another crucial factor in measuring the deadliness of a public health threat is the years of life that it robs from its victims. In the words of the CDC, “the allocation of health resources must consider not only the number of deaths by cause but also by age.” Hence, the “years of potential life lost” has “become a mainstay in the evaluation of the impact of injuries on public health.”
This doesn’t mean that younger people are more important than older people, but it recognizes and accounts for the facts that:
- humans cannot ultimately prevent death; they can only delay it.
- there is a material difference between a malady that kills a 20 year-old in the prime of her life and one that kills a 90-year-old who would have otherwise died a month later.
These realities seem to be lost on some prominent medical authorities, like Howard Bauchner, the editor-in-chief of the Journal of the American Medical Association. He coauthored an editorial comparing 100,000 deaths from C-19 “to the number of U.S. soldiers killed in World War I or in the Korean and Vietnam wars combined.” This is deceptive because it fails to account for the facts that the average:
- lifespan of U.S. residents is 79 years.
- age of U.S. residents who have died of Covid-19 is about 75 years.
- age of U.S. soldiers killed in Vietnam was 23 years.
While ignoring those facts, Bauchner says that “death seems like it should be an accurate measure of the pandemic’s evolution and effects—the worst outcome, an unequivocal outcome.” Given that death is ultimately everyone’s outcome, it is a flawed measure of the pandemic’s severity because it is incomplete.
A much more complete measure of C-19’s lethality also includes the years of life lost by each victim. Yet, determining this is not a simple matter of subtracting their ages at the time of their deaths from the average U.S. lifespan. This is because:
- the average U.S. lifespan includes the deaths of young people, which drives this figure down relative to what it is for older people. So even though the average life expectancy from birth is 79 years, people who are 79 years old live an average of 10 more years.
- C-19 is more deadly to people with preexisting health problems, and these people have lower average life expectancies than healthy people of the same ages.
Based on the average life expectancies of people of different ages and the ages of people who have died from C-19, Just Facts calculates that C-19 robs an average of 13.2 years from each of its victims. This is an overestimate because it does not account for preexisting health conditions.
Even based on the exaggerated figure of 13.2 years, the average years of lost life for each person who dies of C-19 is much less than other common causes of untimely death. For example, accidents rob an average of 30.6 years of life from each victim, while suicides take an average of 35.6 years. And once again, these deaths occur every year, while C-19 is unlikely to have an ongoing high death toll because of its vulnerability to antibodies and limited ability to mutate.
At a March 30, 2020 White House press conference, Dr. Deborah Birx, a world-renowned immunologist, presented a slide of projections for C-19 fatalities based on “five or six international and domestic modelers from Harvard, from Columbia, from Northeastern, from Imperial who helped us tremendously.” The model projected that 100,000 to 240,000 deaths would occur if Americans followed social distancing and hygiene guidelines. Birx added that “we really believe and hope every day that we can do a lot better than that because that’s not assuming 100% of every American does everything that they’re supposed to be doing, but I think that’s possible.”
The upper limit of Birx’s death estimate has been greatly surpassed, but even if two million U.S. residents eventually die from C-19 with 13.2 years of lost life per person, the disease will rob 26.4 million years of life from all Americans who were alive at the outset of 2020. In comparison, the flu will rob them of about 35 million years, suicides will rob them of 132 million years, and accidents will rob them of 409 million years:
Those figures reveal that accidents are about 15 times more lethal to Americans than this nightmare scenario for Covid-19. Likewise, the flu is about 35% more lethal, and suicides are about five times as lethal. This is a substantially more comprehensive measure of deadliness than the tally of lives lost during a year—or any other random unit of time—because it accounts for the entirety of people’s lives and the total years of life that they lose.
It is important to realize that some people experience long-term adverse effects from non-fatal cases of C-19, but this is also true of accidents, suicide attempts, and the flu.
Death Rates
On March 3, 2020, the Director-General of the World Health Organization announced that “about 3.4% of reported Covid-19 cases have died,” and “by comparison, seasonal flu generally kills far fewer than 1% of those infected.” Media outlets widely reported those figures and lambasted President Trump for saying, “I think the 3.4% is really a false number” and “I would say the number is way under 1%.”
Several days later on March 11, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, told a U.S. congressional committee that the mortality rate of C-19 is “somewhere around 1%, which means it is 10 times more lethal than the seasonal flu.”
Contrary to the statements of the World Health Organization and Fauci, Oxford University’s Center for Evidence-Based Medicine estimated in March 2020 that the C-19 fatality rate was far lower and ranged from 0.17% to 0.25%. By October 2020, the Center had slightly revised the range to “somewhere between 0.1% and 0.35%.” This is well below 1%, just as Trump stated. Also, it is nowhere close to 10 times the flu fatality rate, which has averaged about 0.15% over the past nine years in the United States.
In September 2020, the CDC published age-specific estimates for Covid-19 fatality rates that align with the findings of Oxford’s Center for Evidence-Based Medicine. According to the “best” estimates of this CDC report, the C-19 fatality rate is:
- 0.003% for people aged 0–19 years.
- 0.02% for people aged 20–49 years.
- 0.5% for people aged 50–69 years.
- 5.4% for people aged 70+ years.
The last of those figures, which concerns the elderly, was corroborated a month later by a study in the journal Clinical Infectious Diseases. It found that Danes aged 70 and above had a C-19 fatality rate of 5.4%. Likewise, The Lancet published a study in April 2021 that estimated the C-19 fatality rate to be 4.3% to 7.4% among people aged 65 and older in Geneva Switzerland.
Distinguishing between elderly people who live in different settings, the European Journal of Epidemiology published a study in March 2022 which found that the median C-19 death rate in high-income countries was:
- 4.0% among all elderly people.
- 2.2% among elderly people who live in separate settings like houses, as opposed to group settings like nursing homes.
Examining the differences among nations, the European Journal of Clinical Investigation published a paper in March 2021 which found that the C-19 fatality rate:
- is about 0.15% on average for the world.
- “varies substantially across continents and countries.”
- “may be ~0.3%–0.4% in Europe and the Americas (~0.2% among community-dwelling non-institutionalized people) and ~0.05% in Africa and Asia (excluding Wuhan).”
Since publishing its 3.4% fatality rate, the World Health Organization has come to grips with reality on this issue. In January 2021, the Bulletin of the World Health Organization published a study that estimated the fatality rate for C-19 to be 0.23%—or about 1/15th of its original estimate. This new figure is right in the middle of the range estimated by Oxford’s Center for Evidence-Based Medicine (0.1% to 0.35%).
Furthermore, the five studies above all rely on a methodology that tends to overstate fatality rates. This involves using antibody tests to estimate how many people have had Covid-19, but as documented in an August 2020 paper in the journal Cell, the number of people who have had C-19 is “probably significantly higher than antibody tests have suggested.” This means that the actual fatality rates may be lower than found by these studies.
In August 2020, Cambridge University Press published a paper analyzing why early coverage of the C-19 fatality rate was so inaccurate. The study found that purveyors of inflated mortality rates likely confused two different measures of mortality called the “case fatality rate” and the “infection fatality rate.” The first of these is the rate of death among confirmed cases of the disease, while the second is the rate among everyone who had it, including those who were asymptomatic or never diagnosed with it. The paper notes that this misinformation about the death rate “helped launch a campaign of social distancing, organizational and business lockdowns, and shelter-in-place orders.”
Those exaggerated death rates—according to the Bulletin of the World Health Organization—can be traced to “early data from China” suggesting “a 3.4% case fatality rate and that asymptomatic infections were uncommon.” This misled scientists to believe that “the case fatality rate and infection fatality rate would be about the same.”
Notably, the cited source of that claim is a February 2020 report by a “joint mission” of the World Health Organization and the government of China. It wrongly asserts that “the majority of the relatively rare cases who are asymptomatic on the date of identification/report went on to develop disease.”
The implications of that falsehood and how it would impact calculations of the fatality rate are highlighted by a study published by the journal Clinical Infectious Diseases in November 2020. It estimated that only 13% of all C-19 infections that occurred the U.S. from the outset of the pandemic through September 2020 were “recognized and reported.”
Nevertheless, a “fact checker” called PolitiFact published an article in August 2021 which ignored all asymptomatic and unreported cases to calculate that the U.S. fatality rate for Covid-19 is 1.7%. Facebook then used this childish article to censor genuine facts about this issue.
Similarly, media outlets routinely reported the World Health Organization’s initial overblown death rate, even though ample evidence had already undercut it. This is proven by the remainder of this section, which is word-for-word from an article published by Just Facts on March 17, 2020:
Initial media reports of a 2–3% mortality rate for Covid-19 are inflated, and the actual figure may be closer to that of the flu, which has averaged about 0.15% over the past nine years in the United States. A large degree of uncertainty surrounds this issue due to the same factor that prevents accurate counts of infections: unreported cases.
As explained by Dr. Brett Giroir—who has authored nearly 100 peer-reviewed scientific publications and serves as the Assistant Secretary for Health at the U.S. Department of Health and Human Services—the Covid-19 death rate is “lower than you heard probably in many reports” because the bulk of people who contract coronavirus don’t get seriously ill, and thus, many of them never get tested.
Giroir calls this a “denominator problem” because if you’re “not very ill, as most people are not, they do not get tested. They do not get counted in the denominator.” Giroir’s best estimate is that the mortality rate is probably “somewhere between 0.1% and 1%.” This “is likely more severe in its mortality rate than the typical flu” rate of 0.1% to 0.15%, “but it’s certainly within the range.”
Giroir’s estimate accords with a February 2020 commentary in the New England Journal of Medicine by Fauci and others:
A prime example of how journalists misreport on this issue is a March 12th article in Business Insider by Andy Kiersz. In this piece, he compares the “death rates” of Covid-19 from the South Korean CDC to that of the flu from the United States CDC. Based on these numbers, he reports that “South Korea—which has reported some of the lowest coronavirus death rates of any country—still has a COVID-19 death rate more than eight times higher than that of the flu.”
What Kiersz and his editors fail to understand is that the denominator for the Korean rate is the number of “confirmed cases,” while the denominator for the U.S. rate is based on a “mathematical model.” The CDC clarifies how the model works by citing a study on swine flu, which multiplies “43,677 laboratory-confirmed cases” of the disease by 41 to 131 times to calculate the denominator for the death rate. In the authors’ words, they do this because confirmed cases are:
Put simply, Covid-19 death rates that are based upon reported or confirmed infections grossly undercount the number of people with the disease. This, in turn, makes the death rate seem substantially higher than reality.
Transmissibility
Photo credit: iStock/2K Studio
Another important factor in weighing the risks posed by Covid-19 is its transmissibility, or how contagious it is. In this respect, Covid-19 is much more dangerous than the seasonal flu because it spreads much more quickly and widely.
Scientists measure contagiousness with a basic reproduction number, which is the average number of people who tend to catch a disease from each person who has it. This measure is an innate characteristic of the disease because it doesn’t account for actions that people take to prevent it. A February 2020 paper in the Journal of Travel Medicine explains that any disease with a basic reproduction number above 1.0 is likely to multiply over time.
The same paper evaluates 12 studies of the basic reproduction number of Covid-19 in various nations and finds that they “ranged from 1.4 to 6.49,” with an average of 3.28 and a median of 2.79. Based on their analysis of these studies, the authors conclude that the basic reproduction number of C-19 will likely prove to be “around 2–3” after “more data are accumulated.”
In comparison to the flu, a 2014 paper in the journal BMC Infectious Diseases analyzes 24 studies of the seasonal flu and finds that the median result for the basic reproduction number is 1.28. The authors stress that the seemingly small difference between 1.28 and higher figures like 1.80 “represent the difference between epidemics that are controllable and cause moderate illness and those causing a significant number of illnesses and requiring intensive mitigation strategies to control.”
All of the facts above were published in scientific journals by February 2020—but in direct contradiction to them—the Director-General of the World Health Organization gave a press conference on March 3 in which he stated that “Covid-19 spreads less efficiently than flu.”
A range of media outlets echoed that dangerous falsehood, as they did with others from the World Health Organization about immunity and fatality rates. Then with no apparent regard for the World Health Organization’s track record of spurious claims, Google/YouTube adopted a policy in May 2020 of censoring people who post content “that contradicts the World Health Organization (WHO) or local health authorities’ medical information about Covid-19.”
The transmissibility of SARS-CoV-2 has become even greater with the advent of Omicron, which has a much higher reproduction number than earlier variants. This makes the task of shielding the vulnerable even more difficult, but it can be done, as detailed in the last section of this article.
Overreactions
Times Square, NY, May 8, 2020 (iStock via Leo Cunha Media)
With Covid-19 or any other contagious disease, there are mortal dangers in overreacting because measures to limit their spread can cost multitudes of lives. Numerous facts have shown that lockdowns, panic, and other responses to the pandemic have done just that. A small sampling of these include the following:
-
The authors of a July 2020 paper in the Journal of the American Medical Association found:
- There is “an alarming trend across the U.S., where community members experiencing a health emergency are staying home—a decision that can have long-term, and sometimes fatal, consequences.”
- In the five states that had the most Covid-19 deaths in March and April 2020, heart disease deaths were 89% above normal, and diabetes deaths were 96% above normal.
- “New York City’s death rates alone rose a staggering 398% from heart disease and 356% from diabetes.”
- A scientific survey commissioned by the American College of Emergency Physicians in April 2020 found that 29% of adults have “actively delayed or avoided seeking medical care due to concerns about contracting” C-19.
- A scientific survey conducted by the CDC in July 2020 found that about 32% of U.S. adults had “symptoms of anxiety disorder” as compared to 8% around the same time last year. The perils of this are underscored by a 2015 meta-analysis in the Journal of the American Medical Association Psychiatry, which found that the overall risk of death among people with anxiety is 43% higher than the general population.
- A study published by the American Medical Association in September 2020 found that 27.8% of U.S. adults had symptoms of depression during the C-19 pandemic as compared to 8.5% before the pandemic. The same 2015 meta-analysis found that depression is associated with a 71% higher risk of death.
- An article published by the Federal Reserve Bank of San Francisco estimated that “more than 20 million jobs” were “swept away” in the early months of the C-19 pandemic. The potential repercussions of this are highlighted by a 2011 meta-analysis in the journal Social Science & Medicine about mortality, “psychosocial stress,” and job losses. It found that “unemployment is associated with a 63% higher risk of mortality in studies controlling for covariates.”
- A scientific survey conducted by the Kaiser Family Foundation in late April 2020 found that 55% of U.S. workers “have lost their jobs or had a reduction in hours or pay as a result of” reactions to C-19. Regardless of whether these losses are brief or sustained, the same 2011 meta-analysis found that the correlation between unemployment and death “is significant in both the short and long term,” lending “some support to the hypothesis and previous findings that both the stress and the negative lifestyle effects associated with the onset of unemployment tend to persist even after a person has regained a job.”
- Federal politicians have enacted six “Covid relief” laws that will cost about $5.3 trillion, or an average of $41,036 per U.S. household. This has played a key role in driving the national debt to the highest portion of the U.S. economy in the nation’s history. A broad range of facts show that this can have serious negative consequences, including lower wages, weak economic growth, increased inflation, higher taxes, reduced government benefits, or combinations of such results. These, in turn, impair people’s quality of life and can reduce their life expectancy.
-
A study published by the journal European Psychiatry in May 2020 found that:
- governments failed to model the “increased short-term and long-term mortality” caused by the mental health impacts of Covid-19 mitigation strategies like social distancing and lockdowns.
- these actions increased “suicide, depression, alcohol use disorder, childhood trauma due to domestic violence, changes in marital status, and social isolation.”
- the average person in Switzerland will lose an average of about 0.205 years of life due to these mitigation measures.
- “this loss would be entirely borne by 2.1% of the population, who will suffer an average of 9.79” years of life lost.
- these figures are “likely to underestimate the true impact of the mitigation strategies,” and more life may be lost due to “economic adversity, changes to activities of daily living such as eating, sleeping, smoking and ordinary alcohol consumption, or decrease in medical provision to those who have health problems unrelated to Covid-19.”
- A study published by Just Facts in May 2020 found that anxiety related to C-19 will ultimately destroy more years of life than can possibly be saved by lockdowns. With regard to this study, the accomplished psychiatrist Joseph P. Damore, Jr. wrote that it “thoroughly answers the question about the cure being worse than the disease.”
- A study published by the U.K. National Health Service in March 2021 found that at “the start of the Covid-19 pandemic, we saw a sharp reduction in the number of people being referred urgently with suspected cancer from primary care and screening programs.” The problem with this, as explained in the study, is that “early diagnosis is the key to our survival efforts—it means an increased range of treatment options, improved long-term survival and improved quality of life.” Referrals recovered to 107% by December 2020, but not for all cancers, and there is no way to recover the lost treatment time early in the pandemic.
- In March 2021, the journal Frontiers in Public Health published a paper by Dr. Ari R. Joffe, a Canadian medical professor and working physician who was “a strong proponent of lockdowns when the pandemic was first declared.” He went into great detail about “why I changed my mind” and how he and many others were misled into supporting lockdowns by “group hysteria,” “virtue signaling,” and the human tendency to “adhere to our initial hypothesis, and disregard evidence that disproves our favorite theory.” That shortsighted mob mentality, he explained, failed to properly consider the “collateral damage” from lockdowns,” including “severe losses to current and future wellbeing from unemployment, poverty, food insecurity, interrupted preventive, diagnostic, and therapeutic healthcare, interrupted education, loneliness and deterioration of mental health, and intimate partner violence.”
These facts prove that overreacting to C-19 can ultimately kill more people than are saved. Calling attention to this point, a study published by the journal Disaster Medicine and Public Health Preparedness in June 2020 found:
The implications of overreacting to Covid-19 or any other potential hazard are aptly summarized in a teaching guide published by the American Society for Microbiology. This book explains why “the factors driving your concept of risk—emotion or fact—may or may not seem particularly important to you,” but they certainly are because “there are risks in misperceiving risks.”
A Look Back & The Path Forward
Photo credit: iStock/flyparade
On March 31, 2020—as more than 100 nations were implementing lockdowns with slogans like “15 Days to Slow the Spread”—Just Facts published the following words and facts that support them:
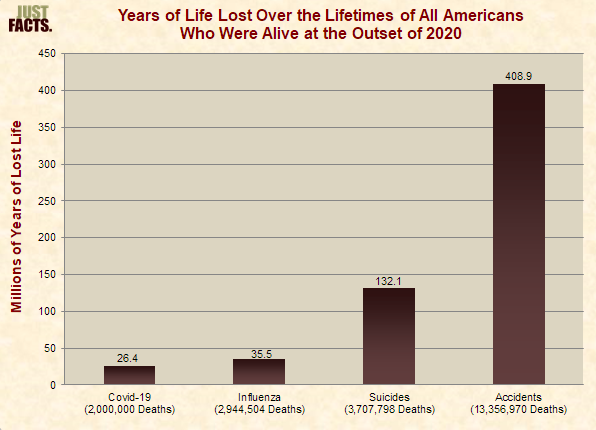
A slew of lethal outcomes over the ensuing months proved that statement true, especially the global number of C-19 deaths per day:
A sample of articles from the New York Times as lockdowns were loosened in the second half of 2020 shows that this carnage occurred across the globe and took many people by surprise:
- July 24: “As the pandemic continues to grow around the world … troubling resurgences have hit several places that were seen as models of how to respond to the virus,” such as Hong Kong, Spain, and Australia.
- July 29: “After months without a single coronavirus death, or even a confirmed case of local transmission, a new outbreak has struck Vietnam. And it’s spreading.”
- October 17: “When the coronavirus began sweeping around the globe this spring, people from Seattle to Rome to London canceled weddings and vacations, cut off visits with grandparents and hunkered down in their homes for what they thought would be a brief but essential period of isolation. But summer did not extinguish the virus. And with fall has come another dangerous, uncontrolled surge of infections that in parts of the world is the worst of the pandemic so far.”
- October 28: “But with countries like France, Italy and Britain reporting their highest death toll in months, and Germany facing soaring cases this week, the authorities are now scrambling to reimpose drastic measures to curb a surge in infections and hospitalizations that could result in more deaths than during the first wave of the pandemic.”
- December 4: “We now know that the second wave in Europe has become deadlier than the first.”
All of this was predicted and predictable. Even the Imperial College of London, which provided the impetus for mass lockdowns, admitted in March 2020 that the “more successful a strategy is at temporary suppression, the larger the later epidemic is predicted to be in the absence of vaccination, due to lesser build-up of herd immunity.”
Making a similar point eight years before the pandemic, a 2012 paper in the journal PLoS One about “Immunity in Society” noted that:
Equally, if very few people are immune to a disease, they can transmit it to others instead of blocking it. Without a potent vaccine, the only way people can become immune to C-19 is by catching it and recovering. This means that too much social distancing may cause more deaths because young, healthy people—who would otherwise catch the disease, recover quickly, and become firewalls—remain as potential carriers.
Quantifying those dynamics, a study published by the British Medical Journal in October 2020 found these stunning and “counterintuitive results” about lockdowns in the United Kingdom:
- The advice given to UK policymakers was focused “on reducing total number of cases and not the number of deaths.”
- “Contrary to popular perception,” the Imperial College paper that was used to justify the lockdown never “specifically modelled” the lockdown.
-
When adjusted to reflect high transmissibility of C-19, the Imperial College model projects that once some basic preventative measures are in place like quarantining infected people and social distancing for the elderly:
- the “closure of schools and universities would increase the total number of deaths.”
- “general social distancing” of the entire population “was also projected to increase the total number of deaths.”
- “postponing the spread of Covid-19 means that more people are still infectious and are available to infect older age groups, of whom a much larger fraction then die.”
Those outcomes assume a C-19 mortality rate of 1% (higher than reality) and that widespread vaccination does not occur for 800 days (slower than reality), but the basic point remains the same: Lockdowns to control the spread of C-19 can actually cause more C-19 deaths by preventing the development of herd immunity among healthy people—the vast majority of whom are very resilient to the virus.
And that only accounts for added C-19 deaths. In addition, lockdowns trigger hordes of other types of deaths both immediately and in the long-term by causing anxiety, depression, missed medical care, unemployment, and poverty.
Despite those facts, media outlets have often scorned the idea of herd immunity, like this October 2020 article in the New York Times which claimed:
That statement suffered from two fatal flaws:
- It was not true that “nearly everyone in a population” must catch C-19 to achieve herd immunity. Even simplistic models—which assumed that immunity is evenly distributed and that all age groups take the same precautions—estimated that herd immunity to the original SARS-CoV-2 virus would emerge when about 50–67% of the population became immune. Using more realistic scenarios, an August 2020 paper in the journal Science placed this figure at roughly 43%.
-
The claim that 85–90% of Americans were still susceptible to C-19 is not based on substantially “different scientific methods” but only on studies that only test for antibodies, which can greatly understate immunity. As documented by the authors of a study conducted in Sweden and published by the journal Cell in August 2020:
- “Our results indicate that public immunity to Covid-19 is probably significantly higher than antibody tests have suggested.”
- Most studies of C-19 immunity merely test for antibodies, but “antibody responses are not detectable in all patients, especially those with less severe forms of Covid-19,” and this is the case with “most people” who catch C-19.
- T cells—which are a key source of lasting immunity—are present in the vast majority of people who have had C-19, and these cells respond like “those observed in the context of successful vaccines, suggesting that natural exposure or infection may prevent recurrent episodes of severe Covid-19” in people who don’t have antibodies.
- Nearly “twice as many exposed family members and healthy individuals who donated blood during the pandemic generated memory T cell responses versus antibody responses, implying that” testing for antibodies “has underestimated the extent of population-level immunity” for C-19.
Collectively, these data indicate that herd immunity could have been achieved with much less loss of life than has occurred. That would have required doing more to protect vulnerable people and allowing young healthy people greater freedom instead of locking them down. This is precisely the opposite of what certain high-profile media figures called for and what most government officials did.
The most lethal blunder of public health authorities has been their failure to protect the people at greatest risk from Covid-19. Despite widespread masking, social distancing, cleaning protocols, and even isolation, SARS-CoV-2 has torn through nursing homes, hospitals, and assisted living facilities, leaving a trail of death and destruction.
Most of that suffering could have been prevented and can be quickly ended going forward with an affordable and time-tested technology called ultraviolet air disinfection. This tech has been proven to stop the transmission of contagious respiratory diseases in settings like hospitals for more than 80 years, but based on a sophomoric misunderstanding about how Covid-19 spreads, the CDC relegated it to a “supplemental treatment” when “options for increasing room ventilation and filtration are limited.”
In September 2021, Just Facts documented the life-saving capacity of ultraviolet air disinfection and promoted it to scholars, politicians, journalists, and commentators. However, most of them ignored the research while big tech suppressed it, thus costing countless lives. Seven months later in April 2022, the New York Times published an essay near the top of its home page by three professors who specialize in disease transmission declaring that ultraviolet air disinfection systems are “highly effective” in preventing the spread of Covid-19 and should be immediately deployed. They finish their essay by asking, “What are we waiting for?”
Another much-needed course correction in the battle against C-19 is better vaccines. Even Fauci and two coauthors confessed this in a commentary published by the New England Journal of Medicine in December 2021 in which they wrote, “The limitations of SARS-CoV-2 vaccines suggest that they will ultimately need to be replaced by second-generation vaccines that induce more broadly protective and more durable immunity.” More than four months later, a Google search revealed a total of zero major national media outlets that reported Fauci’s admission.
Contrary to the rosy picture painted by governments, the media, and big tech, the current crop of Covid-19 vaccines have serious shortcomings, such as these:
- They are injected into muscles, which produces little-to-no immunity in the upper respiratory tract where SARS-CoV-2 enters the human body and first establishes infections.
- They target only one area of the virus called the “Spike protein,” while naturally acquired immunity targets the entire virus.
- They trigger an immune reaction to only a few Spike variants, while naturally acquired immunity attacks a diverse array of Spike variants.
Conclusion
During a March 14, 2020 press conference, U.S. Surgeon General Jerome Adams asserted that “this situation will last longer, and more people will be hurt” if “we are complacent, selfish, uninformed,” and if “we spread fear, distrust, and misinformation.” Yet, that is exactly what many media outlets, governments, and big tech companies have done.
Conversely, Adams said that “we will overcome this situation” if we “pitch in” and “share the facts.”
The essential facts above confirm the wisdom of his words.